The Content and Origin of this Effort
The Robert Wood Johnson Foundation (RWJF) is striving to build a national Culture of Health that will enable all to live longer, healthier lives now and for generations to come, with a strong focus on dismantling structural racism in the U.S. health system. The goal of RWJF’s leadership investments is to ensure that leaders in every community work inclusively so that everyone has a fair and just opportunity for health and well-being.
For 50 years, the Robert Wood Johnson Foundation has operated a powerful leadership development program, Clinical Scholars, possibly the longest-running and most influential clinical leadership program in the country for advancing health equity. Many leaders in healthcare today attribute at least part of their success as leaders to the Clinical Scholars program.
Yet even with recognition of the program’s benefits to leaders, there was a growing sense within RWJF that a new approach to leadership is now needed. That recognition is based on RWJF’s deepened commitment to dismantling structural racism in the health system and a growing recognition that this large, complex, and deeply embedded structural challenge requires more diverse groups of people leading together in new ways.
As we’ve talked with 61 leaders, patient advocates, and patients themselves across the health system (and consulted in open sessions with hundreds more stakeholders), our sense has only deepened that we need fundamental shifts in our thinking about leadership. What we’ve heard about that leadership and the need for a new direction for our long-standing program is the focus of this website.
We are now evolving our flagship leadership program to ensure that it supports leaders to take on the deep, challenging, long-term work of dismantling structural racism in the U.S. health system. This website contains the key learning from our journey of discovery about what kind of leadership we need to achieve this audacious goal.
Project Personnel
RWJF Team
Deborah Bae, Deputy Director, Program
Dee Colello, Deputy Director, Operations, Leadershop for Better Health
Kaytura Felix, Managing Director, Program
Sallie George, Program Officer
Consulting Team
Heather Equinoss, Consultant
Issac Carter, Consultant
Karen Proctor, Strategic Advisor
Luzette Jaimes, Consultant
Melissa Darnell, Project Manager
Russ Gaskin, Lead Consultant
Sharon A. Simms, Consultant
Tema Okun, Strategic Advisor
Advisory Team
Aletha Maybank, MD, MPH, Chief Health Equity Officer, SVP, American Medical Association
David Ansell, MD MPH, SVP for Community Health Equity, Rush University Medical Center
Linda Burnes Bolton, DrPH, RN, Senior VP and Chief Health Equity Officer, Cedars Sinai
Michellene Davis, Esq, President and CEO, National Medical Fellowships
Somava Saha, MD, MS, Executive Lead, Well-being and Equity (WE) in the World
Theresa Trujillo, Co-Directora Executiva, Center for Health Progress
Methodology
Who We Talked To
In order to ground our inquiry in the lived experiences of people within and around the health system, CoCreative conducted 61 in-depth interviews with health system stakeholders, both those who most impact health outcomes and those who are most impacted by disparate outcomes based on race.
The stakeholders were from rural, Indigenous, urban, and suburban communities, and represented a diversity of racial and ethnic identities. Of the people interviewed, 75% self-identified as female, reflecting the heavy representation of women in the health sector. Interviews were conducted virtually via Zoom. Each lasted from 60 to 90 minutes and sessions were recorded and transcribed to ensure accuracy. The stakeholders included:
- 25 people working within healthcare systems, including health system leaders, health educators, leaders at professional health organizations, doctors, nurses, occupational therapists and mental health professionals;
- 31 people in the wider health system including staff of community-based organizations, patent advocates, community organizers, regulatory agencies and professional health associations; and
- 5 patients who have organized, advocated, or been involved in power-building work to create changes within health systems.
The interviewees included 8 clinicians who had participated in, or are currently participating in, RWJF leadership programs.
Some interviews, such as those conducted with patients about their experiences with racism, used an empathy interview format, in which we focused less on analysis of the system and more on their direct experiences, how those experiences impacted them, what meaning they made from those experiences, and how they responded. Other interviews used a “system dynamics” interview format, in which we asked people to consider how and where structural racism is showing up in the U.S. health system and what resources, opportunities, and barriers they see to dismantling it.
CoCreative and RWJF held six consultation sessions with an additional 150 health system stakeholders and patients. In these sessions, which were open to any interested person and promoted through social media and RWJF’s network, participants shared their feedback on the emerging analysis of structural racism, their hopes and aspirations for an equitable health system, and their recommendations for where to focus structural work for the greatest impact. Along with the interviewees, their insights and feedback on our landscape analysis and program pathways are reflected throughout this report.
Additionally, CoCreative and RWJF formed a six-person Advisory Team to challenge and guide thinking on the project approach, assumptions, and learning along the way. The Advisory Team served as the core focus group for testing and refining the project framework and, most importantly, provided framing of both the issues of structural racism in the health system and an articulation of the system we need and want.
- 61 in-depth interviews with health system stakeholders from rural, Indigenous, urban, & suburban communities
- A broad diversity of racial and ethnic identities
- 75% self-identified as female
- 25 people working within healthcare
- 31 people in the wider health system
- 5 patients or patient advocates
- 8 clinicians who had participated in, or are currently participating in, RWJF leadership programs
- 150 additional stakeholders participated in open consultation sessions
When We Talked To Them
CoCreative began interviewing health stakeholders in late August, 2021 and concluded the interviews in mid-December, 2021.
The stakeholder consultation sessions were timed for key intervals in the research process when the insights and feedback from those meetings could most powerfully inform the emerging analysis of the U.S. health system, identify and prioritize structural intervention points, co-create a vision for the kind of leadership that is needed to achieve our goals, and shape the possible program pathways found in our final recommendations.
We offered a $75 honorarium to each interviewee as well as anyone who attended each stakeholder consultation session.
How We Engaged Stakeholders
To guide our inquiry about the challenge of structural racism in healthcare and effective practice in the healthcare and leadership development fields around structural racism, CoCreative developed and utilized interview guides specific to stakeholder segments:
- System Leaders who are leading organizations and/or structural change initiatives related to structural racism in the health system;
- System Analysts who are observing and/or researching the challenge of structural racism in the health system;
- Patient and Patient Advocates who have experienced and/or advocated to remedy structural racism in the health system.
This consultation process allowed us to develop a shared picture of the role structural racism has played and continues to play in the U.S. health system, collect insight on where the most powerful intervention points might be, and understand how health system leaders are experiencing the system around them. Our empathy interviews with patients and patient advocates grounded the analysis and program pathway design in real human experiences and complemented our systems perspective. We shared, socialized, tested and shaped our project goal, definitions, analysis and recommendations with others, expanding our circle of connections over time to build growing alignment about the why, who, what and how of this project.
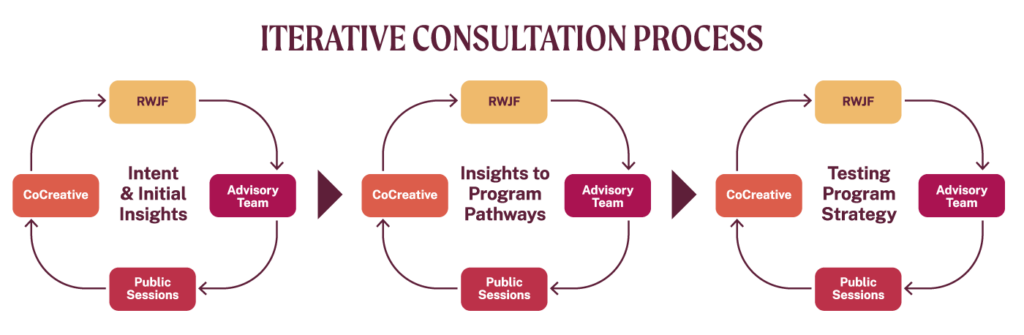
As this graphic illustrates, we designed and followed an iterative consultation process that involved the CoCreative consulting team, RWJF, the project Advisory Team, and public stakeholder sessions. At every point we tested and refined the emerging thinking and analysis, incorporating the insights and feedback of everyone in every cycle.
Definitions
Structural Racism
“A system in which public policies, institutional practices, cultural representations, and other norms work in various, often reinforcing ways to perpetuate racial group inequity.”
– The Aspen Institute Roundtable on Community Change, 2000
“It identifies dimensions of our history and culture that have allowed privileges associated with “whiteness” and disadvantages associated with “color” to endure and adapt over time. Structural racism is not something that a few people or institutions choose to practice. Instead, it has been a feature of the social, economic and political systems in which we all exist.”
Leadership
Leadership is a collective and social process whereby individuals move themselves and others through a process of development and change to achieve health equity with and for people that have been most marginalized.
Healthcare System
The “healthcare system” centers on clinical care delivery. It includes the hospitals, doctors, nurses, technicians, support staff, and administrators who run healthcare institutions, along with the payment systems, insurers, technology providers, and others who support clinical systems.
Health System
The term “health system” refers to the much larger system that comprises all the people, organizations, institutions, and resources that contribute to maintaining and improving health. This larger system includes many more actors and institutions across the public, private and nonprofit sectors.
Whom We Consulted
The quotes from this site came from interviews with 61 stakeholders across the health system, 6 Advisory Team Members, 17 RWJF staff members, and 148 other stakeholders who provided feedback and input through our open consultation sessions.
Appreciations
We recognize that the work to understand and address systemic racism is ongoing and continually finds its source in the experiences, perspectives, and labor of Black, Indigenous, and people of color. Countless individuals and groups, over generations, have dedicated their lives to the pursuit of equity. We wish to honor the legacy of their work.
We are grateful to the 61 people we interviewed who contributed their wisdom, shared their aspirations, and spoke their truths about how structural racism manifests itself within the health system and what it will take to dismantle it.
We appreciate the work of the Advisory Team members—Theresa Trujillo, Dr. Somava Saha, Michellene Davis Dr. Linda Burnes Bolton, Dr. David Ansell, and Dr. Aletha Maybank—for informing and refining the project intent, the definitions of key terms used throughout the project, the landscape analysis, the leadership program strategy and design, and for their own courageous leadership to bring forward a more equitable health system.
We thank Dr. Miraj Desai for sharing his research, advice, and consultation on the emerging insights from the field.
We are grateful for the collaboration of David Peter Stroh in developing the system maps to analyze systemic racism within the health system.
Finally, we thank the 150 people who attended stakeholder consultations sessions to co-design the collective leadership program.